The microbe can colonize the gastrointestinal tract without hindrance without the normal intestinal microflora. How severe the symptoms are can change in range.
Complete deterioration is the resultant effect of antibiotic therapy leading to C.diffi infection. Those patients are usually hospitalized when they get an infection. Nevertheless, more effective hospital management strategies today have shown an overall decline in cases. However, bacterial illness is diagnosed more often in younger patients outside the hospital. Many of the associated comorbidities increase mortality risk due to infection. These include liver disease, chronic kidney disease, and ischaemic heart disease.

C. diff can also come through several routes, facilitating disease transmission. Moreover, this germ can be impervious to some protective measures. While C. diff infections typically take a mild course, the illness can sometimes be serious and fatal, leading to problems. Diagnosis and intensity of the disease are the main criteria for deciding on treatment. It indicates diagnosis through laboratory tests. The first step in treatment is stopping the drug that was taken when the symptoms occurred. But if it is severe, it will require specialty therapy. With some degree of protection, C. Diff can be prevented. Know more and be more cautious.
The first reported case was published in 1892. The patient had boric acid gastric irrigation — oddly enough, it was not about a course of drug treatment. Subsequently, antibiotic use was linked with a high incidence of pseudomembranous colitis. Infections were tolerated as a problem of antimicrobial therapy well into the last decades of the 20th century, predominantly nosocomial. They had not yet been recognized as a serious threat to the healthcare system. Yet, not long after, the threat posed by the C. diff microbe began to be realized.
When statistics show a high rate of disease recurrence, the other aspect that has affected mortality with the increase in recurrence is also observed. Unsurprisingly, infections were among the top causes of death caused by diarrhea. Increased infection rates could suggest an epidemic spread; some authors mentioned this. Large epidemic outbreaks occurred in the US, Canada, and the UK and peaked in 2004-2006. This bacterial infection has become one of the leading nosocomial infections in the US and other countries. Primary infection risk can be lowered with sanitation control, vaccination, and drug management.
C. diff is an anaerobic toxin-producing bacterium that can cause serious diseases in the human body. This means that the microbe is an anaerobe, so if the infection spreads to a new host, it must have breached a massive barrier of atmospheric oxygen to do so. The bacteria exist outdoors, too. They're normally present in the soil, water, and human and animal feces.
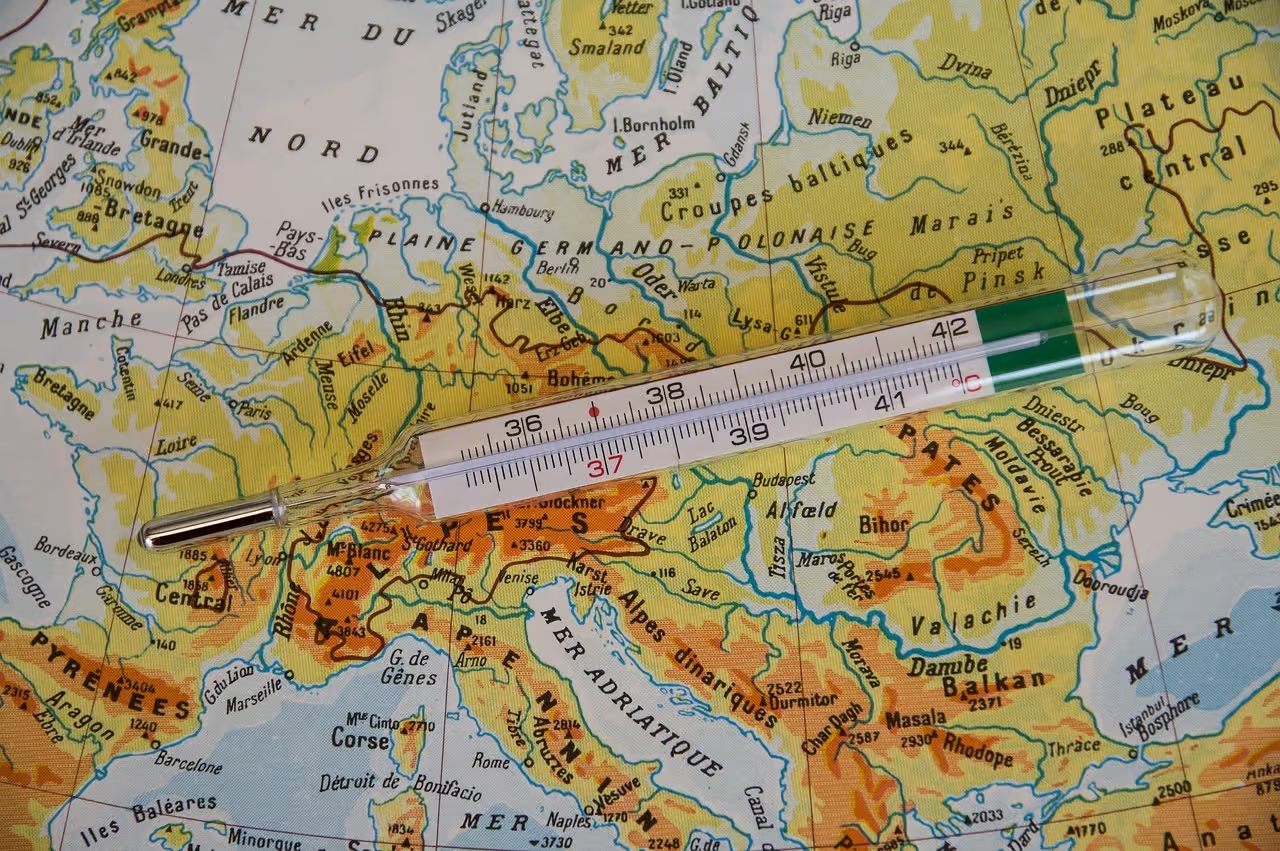
I.e., they can survive at fairly high temperatures. Their optimum growth temperature is about 37 degrees Celsius. The spore form is also resistant to UV, heat, many disinfectants, and drugs, providing a major additional challenge in temperature resistance. Although multiple classes of antibiotics likely cause the disease, Those include penicillin is one of the most commonly used drugs.
On the other hand, there are also some risk factors for C. diff infection. These are generally related to health-related issues and often poor patient conditions. As a result, C. diff infections are extremely frequent in hospitals.
The bacillus particles disseminate quickly in the human intestine tract. The majority of transmission of C.diff pathogen is by the fecal-oral route that is directly associated with poor hygiene. Asymptomatic patients can act as potential reservoirs of C.diff, completely unaware of the infection that they have transmitted. Adults and newly born children can harbor C. diff bacteria. Such strains of bacteria have the highest possible risk of transmission in clinical settings, hospitals, and other medical facilities. Patients and staff can become infected through direct contact with one another.
C. diff is spread from contaminated equipment and commonly used objects. If healthcare workers do not provide optimal care, hospital infections can occur. In hospitals, precautions should be taken, patients should be separated, and hospital fouls should be cleaned; otherwise, the number of C. diff forms will increase. The researchers added that vegetables are another important source due to C. difficile's ability to survive a long time in the environment. The bacteria was detected in several different types of vegetables.

Various strains of Clostridium are present in the environment, such as soil, air, and water. Bad hygiene can spread the infection through contact with contaminated soil or compost. As a result, through contaminated food, the bacteria can penetrate the body. C. diff bacteria can also become airborne. C. diff has also been seen living in vents and on high surfaces in clinical settings. C. diff is commonly found in many different places. Confirmed strains of the bacteria were separated from samples found in parks, shops, and restaurants.
According to C.difficile, bacteria live not only inside humans. The microbe lives in the intestines of dogs, cats, pigs, and birds, so they can also carry it. Pets can become symptomatic when their gut is overwhelmed with Clostridium bacteria, which makes spores in large amounts. However, even asymptomatic infection does not mean pets are not carriers of infection. C.difficile has zoonotic potential and can humanely be transferred from unfavorable conditions or animals to humans. In multiple studies, the presence of dogs in the home has been associated with increased infant colonization rates. Notably, cats showed a higher prevalence of toxigenic strains than dogs.
C. diff is a bacteria that is found in the large intestine. Consequently, symptoms may involve the large bowel, primarily its distal portion. In immunocompetent and healthy individuals, the presence of the bacteria is asymptomatic. The gut microbiome of an otherwise healthy asymptomatic carrier does not differ significantly from that of a non-carrier. C. diff can remain in patients for up to 1 month. Such people are then carriers and can transmit the bacteria. Also, newly born children very often pursue an asymptomatic course. Symptoms are caused by the toxin, for example, clostridial glycosylation exotoxin.
People often experience the symptoms after an drug therapy. By disturbing the equilibrium of normal intestinal microflora and inhibiting certain bacterial communities, antibiotics can subsequently lead to loss of diversity and resistance to colonization in the gut. So, paradoxically, antibiotics, the principal therapeutic agents against various infections, are also a primary risk factor for C. diff infections. The type of antibiotic is not the only important factor; the dose, use of combination therapy, and prolonged duration of the drug therapy also matter.
Symptoms of C. diff infection can be mild to severe. C. difficile can have a broad spectrum of disease, from asymptomatic to toxic megacolon. Recurrent infection is the re-emergence of symptoms two to eight weeks after completing appropriate treatment. Recurrence of the original infecting strain or reinfection with a different strain may lead to recurrent symptoms. We will describe each symptom in detail to help you identify each sign of C. diff infection.

The primary symptom of a mild to moderate infection is watery diarrhea. During C. diff infection, loose motions is primarily observed, which is watery and often with mucus or occult blood. Watery diarrhea consists of stool with a stool that is too loose. It can be semi-liquid, liquid, or watery consistency. Frequent passage of bowel movements is also a feature, and the number of bowel movements, in turn, depends on the individual.
The intensity of the loose motions and whether any other symptoms develop also varies depending on the case. The long-standing watery stool may cause dehydration if the stool is abundant and watery due to diarrhea. A diarrheic patient having a mild or moderate course most often finds mild or moderate loose motions without evidence of systemic infection.
This may be associated with nausea and throwing up. Anorexia can also be a side effect of unpleasant symptoms. As patients feel sick, their bodies are more likely to become weak and tired. Other symptoms and the patient's health differ in each case. Nausea is a very recognizable symptom pointing an uncomfortable sensation in the gut and an enhanced necessity for throwing up. Usually, with nausea, there is pale skin, increased sweating, low pressure, and dizziness.
A mild fever or sub febrile condition occurs in C. diff infection. Fever is an uncommon symptom in fewer than 15% of mild cases. It also occurs infrequently, but high fever may be the symptom in more severe cases. In C.diff infection, ongoing fever and loose motions may lead to dehydration. In children and adults, a sub febrile status corresponds to an increase in body temperature not more than 38 ℃. Increased body temperature is a universal response that turns on for many types of infections.

Diarrhea in C.difficile infection is often associated with diverse forms of belly pain. These are more serious cases in which patients develop the disease acutely, along with diffuse belly pain and abdominal distension. Flatulence is a type of belly fullness most commonly seen after food consumption. In cases of a C. diff infection, the abdomen may be distended. This is due to the inhibition of intestinal motility during the infection.
In more extreme situations, the inflamed intestines. Endoscopy can then detect the characteristic alterations of the colonic endothelium. Acute colitis may be life-threatening when leading to multiple organ failure.
Hypovolemia is the inadequate blood volume in the body's vascular space, ultimately leading to cardiovascular dysfunction. In particularly severe and acute C. diff infection, it can prove dangerous. Septicemia, colonic dilatation, and intestinal perforation with peritonitis can result.
These conditions are problems of serious cases of C. diff infection. Sepsis condition can occur when the body overreacts to bacteria. Sepsis is caused by bacteria that enter the blood circulation. Another serious problem is toxic dilatation of the colon, in which the wall of the intestine becomes inflamed, which affects not only muscle cells but also nerve plexuses connected with peristalsis. Suppose perforation of the intestine occurs, i.e., disruption of the integrity of all layers of the intestinal wall. In that case, the patient is exposed to death or a permanent impairment of health.
Investigations are necessary as they are done when the patients present with classical features of loose motions and other infectious causes are not suspected. Differential diagnosis should also be done with other diseases with similar symptoms. In some cases, additional tests might be needed if none of the tests comes out positive for C. diff.
However, C.difficile infections can follow a path common to diseases like Crohn's Disease, Irritable Bowel Syndrome (IBS), or Salmonella, so doctors must also consider these diseases when diagnosing a patient.
Furthermore, direct mechanisms (such as the osmotic) appear responsible for more antibiotic-related loose motions cases than the commonly postulated disruption of the intestinal microbiota. But if there is diarrhea with colitis, it is almost always a C. diff.

If you have a lot of loose motions, you must do tests. Stool examination and culture are crucial for confirming diagnosis. There are different ways to perform the toxin tests to confirm the bacteria. These methods have a short turnaround time but tend to be ineffective. Their sensitivity is high, but stool toxin concentration is not a reliable discriminator of carrier vs. infection. It is not always easy to diagnose infection as detection does not always mean diagnosis. Furthermore, testing should be avoided if diarrhea is clearly due to other causes, such as the use of laxatives.
Some cases also involve imaging studies. Abdominal and pelvic radiographic imaging or lower gastrointestinal endoscopy. These tests are used in patients with fulminant colitis or the setting of an alternative diagnosis of colitis. The findings will typically be mild and nonspecific in patients meeting the criteria for mild to moderate colitis, in whom belly radiography or CT scans are carried out. Accordingly, imaging studies are not indicated in these patients.
Key points for diagnosing C. diff infection: colonoscopy also plays a role in diagnostic value. Extensive colonoscopy can identify myriad microbes and serve as a proxy for history or severe disease not detected from routine lab tests. Different tests can be useful to confirm the diagnosis and to check how severe the disease is and what problems it has caused.
It is important to deal with cases of C. diff infection by following a multi-step process and with caution. Fighting the microbe can also differ in type, depending on the type of body condition and how bad the disease is. For less severe cases, this will first require stopping the use of the antibiotic responsible for the symptoms.
The initial treatment involves different varieties of drugs, which would depend on the intensity of the C.difficile infection. Drugs with minimal absorption in the intestine are utilized. For non-acute disease, the dosage of antibiotics considers the patient's microbiota and tries to preserve it against the overgrowth of C. diff. In severe cases of colitis, a higher dose of drugs is prescribed.
Antibiotic therapy should be given over 10 days. Drug treatment over days to weeks will rapidly decrease the number of microbes and alter the gut microbiome. It usually takes months, therefore, for the average patient to fully recover from it. Because patients have absolutely no protective buffer during such recurrences, they are very common during this period. Antibiotics are alsonot effectivel because diarrhea leads to gastrointestinal hypermotility, which decreases contact time in the small and large intestines and consequently decreases the effect of antibiotics.

Aside from drug treatment, different therapeutic modalities are used when C. diff infection is treated. In some cases, intestinal irrigation or special enema hydrocolonotherapy is used. This process entails washing out the lumen of the large intrinsic organ with heat-liquified water, washing out food and dried fecal masses, and utilizing it to detoxify the body. The pressurized water gets drawn up through the rectum. In patients with intestinal obstruction, retention enema is indicated to ensure adequate site-directed antibiotics. This way, it is hygienic and does not cause pain.
Recurrences characterize Diarrheal C.difficile infections. Specialized therapy should be employed for recurrences if antibiotics are lacking. In the most extreme circumstances of infection, surgical treatment could be needed to save a patient. Intestinal obstruction is an ominous feature of a deteriorating infection with the potential for bowel necrosis and life-threatening emergency surgical intervention, including fecal microbiota transplantation (FMT). This has been very effective in the treatment of recurrent C.difficile infection.
Adequate preventive measures are crucial because C. diff is one of the top infectious causes of hospital diarrhea. Sanitary control measures take into account rapid identification and isolation of the patients, case room disinfection, and use of personal protective equipment. One of the basic elements of transmission prevention is hand hygiene. This leads to serious long-term consequences, as long-term use of antibiotics is still one of the biggest risk factors. Vaccines are also being studied right now.
Table of Contents