
infection with complications if you do not treat it. Pay attention to the warning signs. It is also important to remember that cellulitis is not the same as cellulite. Although the names are similar, cellulite is natural fatty tissue in a woman's body that gives the skin an orange peel appearance.
Causes
The skin’s job is to protect the body from external factors. Unfortunately, some threats are able to break through this barrier. When harmful microorganisms enter a wound as a result of skin damage, it can lead to infection.
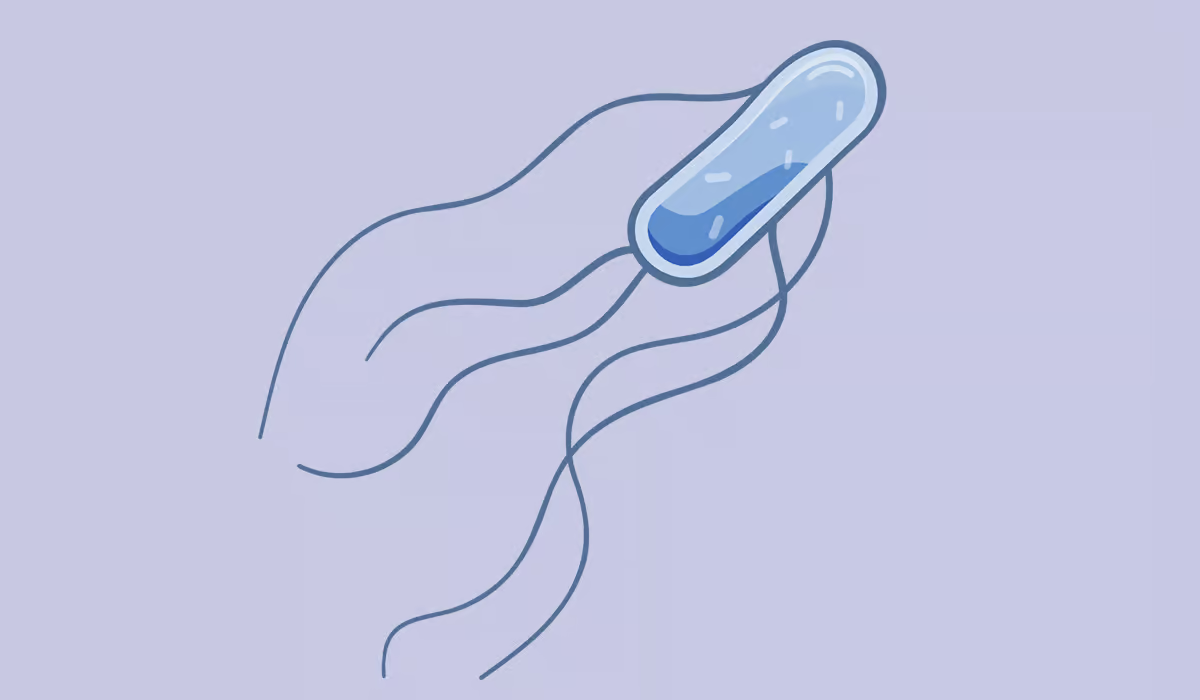
Cellulitis is caused by bacteria. Pathogens penetrate deep into the dermis and surrounding subcutaneous tissue, causing inflammation. The most common causes are streptococci (Streptococcus pyogenes) or Staphylococcus aureus (Staphylococcus aureus).
Some people may be more susceptible to bacterial skin infections. The risk group includes primarily patients with compromised immunity and people suffering from comorbidities such as diabetes or peripheral artery disease. Furthermore, wounds and skin injuries can also increase susceptibility to infection. Therefore, any insect or animal bites, as well as injection punctures and surgical incisions, put you at risk of cellulitis.
This type of skin inflammation is quite common. It most often affects older people. It can also occur in children, but this is much less common. This is probably due to the fact that children’s skin has better regenerative abilities.

Spreading
Cellulitis is not airborne, so it is not classified as a typical infectious disease. However, you should remember that the bacteria causing cellulitis can spread to another person under certain conditions.
Infection will not occur through contact with healthy skin alone. The risk only arises when the other person has any damage to their skin. Even minor scratches, shaving abrasions, cracked skin on the heels, or open pimples can lead to infection. In such places, bacteria can penetrate deeper layers of tissue and cause inflammation.
For this reason, using shared items belonging to a person with cellulitis, such as towels, sponges, or razors, also poses a risk. There is also an increased risk of infection in public places where people walk barefoot or come into contact with damp surfaces. For example, in swimming pools, gym showers, or saunas.
Symptoms
Cellulitis causes distinct skin symptoms. The inflammation develops rapidly. The first symptoms usually appear within 24–48 hours after the bacteria enter through damaged skin. The duration of the infection depends primarily on how quickly treatment begins, the extent of the infection, and the patient’s overall health.
The infected area of skin becomes red, tender, and warmer than the surrounding tissue. Swelling and pain are also common, usually noticeable when the area is touched. Some patients may develop blisters. It is worth noting that, unlike other bacterial infections, cellulitis does not usually cause purulent discharge.

The symptoms are the result of the body’s defence response. Cytokines and neutrophils, which are responsible for fighting pathogens, cause vasodilation and the influx of immune cells, leading to redness and swelling. The skin also produces antibacterial peptides that help fight the infection.
In more advanced cases, bacteria can enter the lymphatic vessels. A red line then appears on the skin, running towards the nearest lymph nodes, which commonly swell. If the inflammation spreads further, systemic symptoms such as fever, chills, headaches, or nausea may occur.
In such a situation, urgent medical attention is necessary, as untreated cellulitis can lead to serious complications.
Diagnosis
To make a diagnosis, the doctor usually begins the visit with an interview and a physical examination, which involves assessing the affected area of skin. They may then order blood tests. Inflammation of the connective tissue causes elevated inflammation markers. CRP and ESR are substances measured in the serum that help assess whether an inflammatory process is occurring in the body. Elevated values may therefore confirm a bacterial infection.
However, to select the appropriate antibiotics for treatment, it is also essential to perform a microbiological test. The doctor takes a swab from the infected areas of the patient’s skin. The test is painless, non-invasive, and uses a cotton swab. It will detect the specific bacteria responsible for the disease.

Treatment
Antibiotic therapy is the basis for the treatment of acute cellulitis. It is important to take the prescribed medication consistently. It may take up to several months for all symptoms to disappear. If the patient interrupts treatment during this time, the cellulitis may return.
Pain therapy is also important. However, in the acute phase of the disease, it is better to avoid NSAIDs, as they can lead to serious complications (necrotising fasciitis). Therefore, other pain-relieving preparations such as paracetamol are usually used. Patients often take this standard medication without a prescription, as it effectively relieves pain and lowers fever.
Patients should also protect the affected area of skin from further injury. If the inflammation affects a limb, it is advisable to keep it elevated, which promotes circulation and reduces swelling.
When cases are severe, doctors treat patients in a hospital, give them antibiotics through an IV, and keep a close watch on their condition. Monitoring the patient’s health is very important, as the disease can lead to serious complications.
Complications
Sometimes cellulitis can spread beyond the original site of infection. In extreme cases, harmful microorganisms can enter the bloodstream, leading to sepsis. The symptoms of sepsis appear suddenly and require immediate medical attention. These include high fever, vomiting, drop in blood pressure, rapid heart rate, and confusion. If sepsis is suspected, seek medical help immediately or go to the hospital, as it is a life-threatening condition and requires hospital treatment.
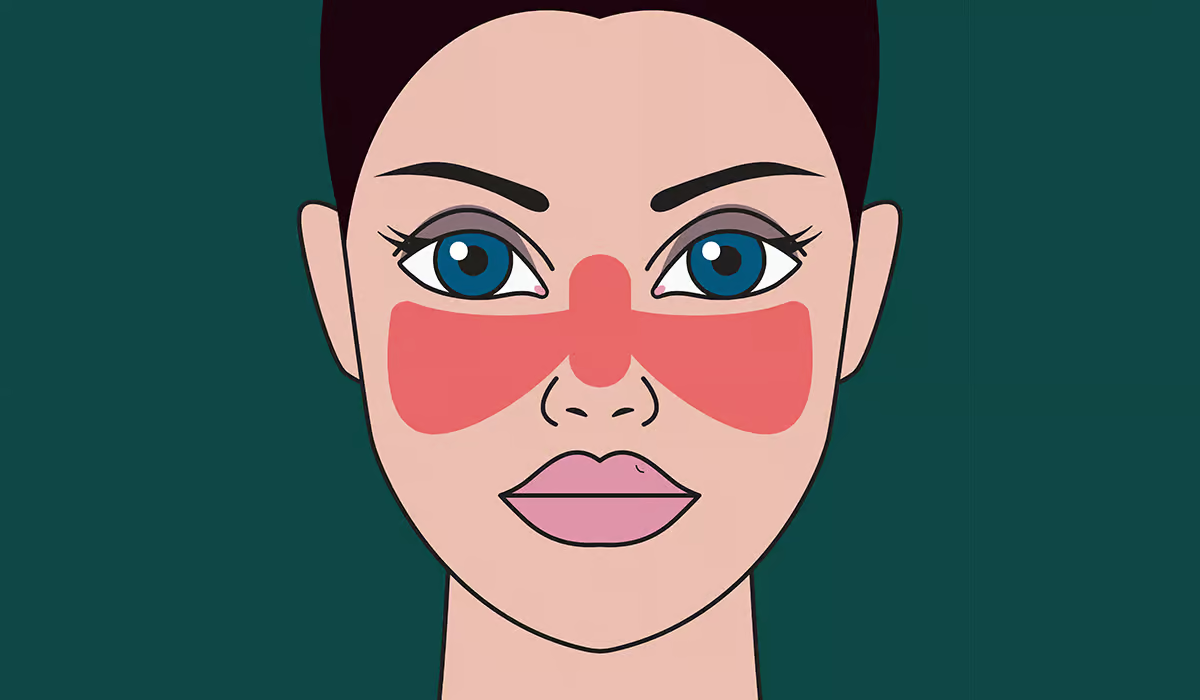
If cellulitis affects the face, especially the nose and forehead, there is a risk that the infection will spread to the meninges and brain. This can lead to meningitis or encephalitis. In such cases, symptoms may include severe headache, neck stiffness, nausea, impaired consciousness, and convulsions. The occurrence of any of these symptoms also requires immediate hospitalisation.
Prevention
The most important thing in preventing cellulitis is taking care of your skin. Keeping it clean and moisturised reduces the risk of harmful bacteria entering the body. Proper hand hygiene is also important. Regular washing with soap and water protects against infections, and when this is not possible, it is worth using disinfectants.
Dry skin increases susceptibility to injury and infection, so it should be moisturised regularly with lotion, especially after a bath or shower. Hands are particularly prone to dryness, so it is a good idea to always carry hand cream with you.

Any skin injury, such as cuts, abrasions, insect bites, burns, frostbite, or scratches, increases the risk of cellulitis. So, exercise caution when gardening, or engaging in any activities that could irritate your sensitive skin. Also, wear protective gloves and keep your nails trimmed to avoid accidental scratches.
If skin trauma occurs, take immediate action: gently wash the wound, apply an antibacterial ointment (if available), and cover with a plaster or bandage. Clean and change the dressing daily until the wound has healed completely.
It is also important to treat underlying skin conditions that increase the risk of infection. These include, among others, athlete’s foot and seborrhoeic dermatitis. Treatment of chronic conditions such as diabetes, eczema, leg ulcers, or peripheral artery disease (PAD) under medical supervision significantly reduces the risk of developing and recurring cellulitis.
Summary
Cellulitis is an acute inflammatory disease of the connective tissue that develops when bacteria enter through damaged skin. Risk factors include chronic diseases (diabetes), a weakened immune system, and skin injuries. Symptoms usually appear quickly and include redness, swelling, pain, and increased skin temperature. To diagnose cellulitis, doctors review the patient’s medical history, examine the skin area, and run blood tests. Treatment primarily involves antibiotics prescribed by a doctor. Avoid sharing personal items and exercise caution in public places. Without proper treatment, bacteria from cellulitis can spread into the bloodstream and lead to sepsis. In such situations, immediate medical attention is necessary.
Sources
- Brandon D. Brown, Kristen L. Hood Watson (2023). Cellulitis. https://www.ncbi.nlm.nih.gov/books/NBK549770/
- Tadhg Sullivan, Eoghan de Barra (2018). Diagnosis and management of cellulitis. https://pmc.ncbi.nlm.nih.gov/articles/PMC6303460/
- Brandon D. Brown, Kristen L. Hood Watson (2023). Cellulitis. https://pubmed.ncbi.nlm.nih.gov/31747177/
- M. N. Norazirah, I. S. Khor, J. Adawiyah, A. M. Tamil, M. N. Azmawati (2020). The risk factors of lower limb cellulitis: A case-control study in a tertiary centre. https://pmc.ncbi.nlm.nih.gov/articles/PMC7136668/
- Julio Collazos, Belen De La Fuente, Alicia Garcia, Helena Gomez, Candela Menendez, Hector Enriquez, Paula Sanchez, Maria Alonso, Jose Guerra, Arturo Artero, Marino Blanes, Javier De La Fuente, Victor Asensi (2018). Factors Associated With Sepsis Development in Cellulitis. A Prospective Analysis of 606 Episodes in Adult Patients. https://pmc.ncbi.nlm.nih.gov/articles/PMC6253918/
- Maddalena Peghin, Elena Graziano, Cristina Rovelli, Paolo Antonio Grossi (2023). Prevention and treatment of recurrent cellulitis. https://pubmed.ncbi.nlm.nih.gov/36853755/
Lymphoma: What Is, Causes, Symptoms, and Treatment

Osteoarthritis: What Is, Causes, Risk Factor, Symptoms, and More
Bird Flu: What Is, In Humans, and In Birds

Hypoglycemia: What Is, Types, Symptoms, and Causes
Trigger Finger: What Is, Causes, Symptoms, and Treatment

Hemoglobin: What Is, Types, and Norms

Anemia: What Is, Causes, Symptoms, and Types
Pancreatitis: What Is, Causes, Symptoms, and More
Bacterial Vaginosis: What Is, Causes, Symptoms and More
Fatty Liver: Causes, Epidemiology, Symptoms, and More
Scarlet Fever: What Is, Causes, Symptoms, and Similar Ailments
C. Diff: What Is, Epidemiology, Transmission, and More
Lupus: What Is, Warning Signals, Diagnosis, and Treatment

Neuropathy: What Is, Symptoms, Causes, and Types
Listeria: What Is, Ways of Infection, Signs, and More
