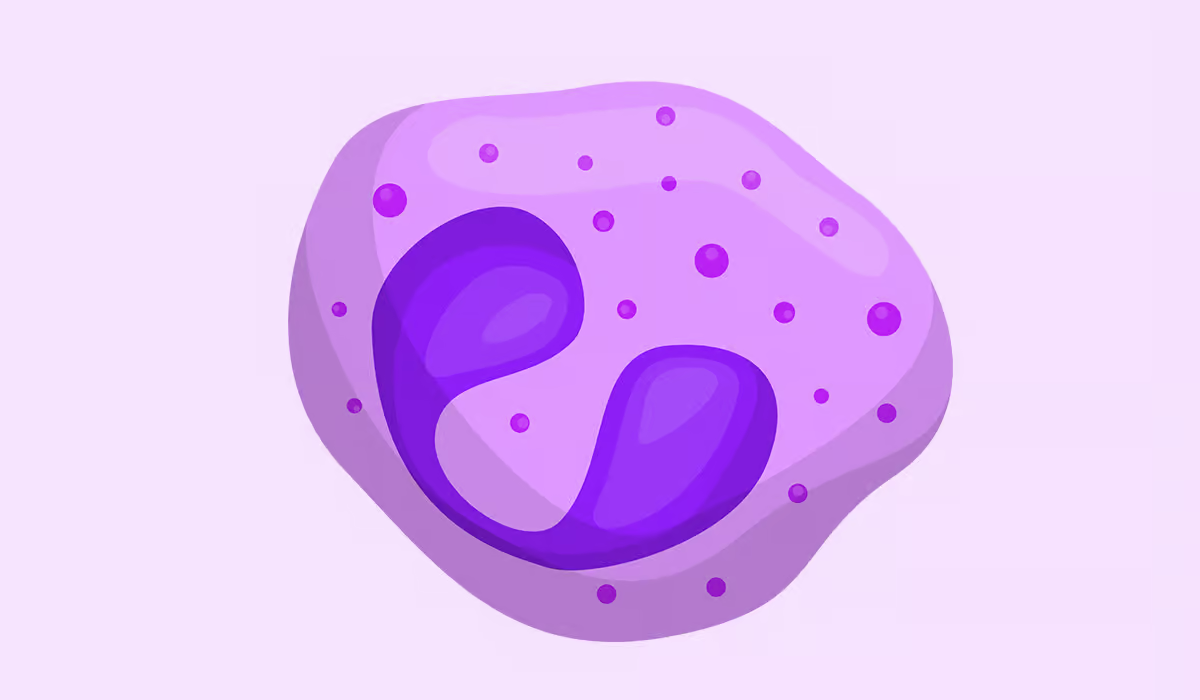
Eosinophils are one of the white blood cell types that are quite unique from the rest of the white blood cells. They participate significantly in the immune system's activity. The cells were first found in the late 19th century. They were named after their affinity for eosin, a red dye used in microscopes. Eosinophils belong to granulocytes which further include neutrophils and basophils as well….
Table of Contents
Disclaimer: The information provided on this website is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition.
© HealthSimple.com 2025 Contact Privacy Policy Terms and conditions Cookie Policy