dysfunction – but has a pathogenesis that primarily encompasses cartilage to joint environment areas, including tendon, muscle, nerve, and other structures, critical to function with joints.
But even before all this, we must find an answer to the question — what are joints? And what is the mechanism of their harm? This is a key aspect of our comprehension of the disease issue. Most of us are unaware that joints are not one bone but rather a nexus between two or more bones that enables the movement of one in the direction of the others. A joint is a mechanical function, so an abnormal mechanical load on a joint can lead to injury. Complicated, but if you don't get it, don't panic. We will go into more detail on this a little later in the text.

Thus, it leads to voice and mobility disability in the elder people. The chance of osteoarthritis advances with age. The disease occurs due to both, internal and external factors. The aging of the U.S. people, coupled with the epidemic of obesity, means that more family physicians will be seeing patients with osteoarthritis.
It affects the knee joint, hand, or hip. It can also affect the spine, feet, and shoulders in some cases. Most diagnoses are made based on the symptoms. There are many different treatments. There exist treatments that are additive and proven to alleviate pain. Find out more about the burden of osteoarthritis.
As per expert statistics provided to us, osteoarthritis is bust in people within the age group of 70 -74 and is as high as 40%. New findings regarding osteoarthritis have also been made by scientists recently. Indeed, while the signature finding and immediate cause of the disease described here is the loss of articular cartilage, OA has increasingly been described as a whole-joint disease that involves all of the reticular structures.
Using the word ‘remodeling,' they also recognize some bone atrophy relatively early on in the course of this disease, which is not a particularly positive finding, but at least researchers acknowledge it. The synovial membrane gets activated and produces more synovial fluid, which causes swelling. There is swelling at the joints of the hind limb, and lack of use further promotes muscle weakness and atrophy. This is pretty much what the disease looks like from the inside.
So, what causes the processes of disease that cause such a thing? Thus, it is the abnormal loading of the joint. Complex systems monitor the action of the internal muscles that contract in synchrony and very smoothly in a healthy young joint, protecting the joint from injury. This leaves them free to move without pain! And the rest of it, the ligaments, all do their job, and they do it well. This yields a distribution of load through the physiologic makeup of the joint during motion in a normal person.
By comparison, in the case of cartilage wear, the loading is heterogeneous. Key components begin to fail and no longer perform their protective functions. The load then causes additional injury and mal-alignment of the moving joint. Muscles may no longer work together in a coordinated fashion, while inflammation in the joint may initiate more changes.

Both endogenous and exogenous risk aspects for osteoarthritis are identifiable. The article emphasizes biological, lifestyle, and socioeconomic factors and their effect on the development of disability due to the disease. Discover the key contributors to risk for this multifaceted illness.
Genetic factors are undoubtedly important, and we, of course, have to note that here. To do this, scientists placed twins in a study. That enabled them to showcase the trait impact of inheritance in hip and knee osteoarthritis. However, only in the rare exception cases can the characteristic disease be traced to the action of one gene. Many different genes interact, making the development and progression of cancer much more closely correlated. Also, genetics, which is not solely a contributing predisposition to these, continues but is also coupled with other risk factors.
As you may have heard, exercise is central to a healthy lifestyle. However, the wrong type of physical work can cause more harm than good. This is why some competitive sports increase the chance of developing osteoarthritis. Those athletes need to look after themselves and not push themselves too far. Thus, only the degree of exertion and excess of practice in sports are related to disease; moderate, regular running provides a slight, pleasant, very small risk.
Sports that seem to have a higher risk of osteoarthritis exposure include American football, for instance, where knee and neck injuries are common. Repetitive joint damage is also a risk with baseball and soccer.
Those who have work that demands a lot of physical movement over-exercise people are at risk! As a result, several workers also fall into the risk category for osteoarthritis. Miners, construction workers, and other laborers are also employed. We feel very sorry for them!
It is also related to jobs that involve kneeling or squatting for longer periods, which pose a higher risk of disease. And since the disease can also occur in other places, like the hands, repetitive motion jobs that require squeezing the thumb and the index or middle fingers together to hold something are a major hindrance to disease progression. In contrast, farmers have been assigned a very high rate of hip osteoarthritis. This study inconsistently associated joint pain in other occupational activities (e.g., climbing stairs or walking on uneven ground) with osteoarthritis.).

A multitude of mechanical traumas may also contribute to the subsequent development of the disease process. Such events comprise hip dysplasia, joint surface fractures, and meniscus and tendon tears. These deleterious events exacerbate joint instability and are thought to precede the development of osteoarthritis. Other risk factors are high body mass, high activity levels, residual insufficiency, or malalignment of the joint. So, after injuries, you need to avoid overloading the injured areas. Keep this in mind.
For years, it was uncertain whether the extra weight came before osteoarthritis or was a result of the deprivation of movement and disability that can come with the disease. However, it is safe to assert that overweight people suffer from osteoarthritis in high numbers. Well, the knees are not particularly good. So, you must act before this disease occurs.
Weight loss decreases the risk of obesity-related osteoarthritis in overweight individuals. But please be careful; this will help you lose some excess weight. This is especially true for overweight people, so caution should be exercised when overloading during an activity. Well, if you plan to exercise, do it in moderation!
Another thing that can impact how you develop osteoarthritis is diet. Not only an unhealthy diet causes obesity. Certain dietary components are particularly important. Those are the so-called oxidants propelling a number of common age-related diseases, such as osteoarthritis. That said, it is a scientific fact that reactive oxygen species inflict damage to cartilage collagen and synovial fluid constituents.
On the other hand, micronutrient antioxidants protect from tissue injury. Consequently, we can hypothesize that a high dietary intake of these micronutrients is protective for OA. So don't deny yourself of whole fruits and vegetables!

It turns out that hormones might play a key role here, too. Higher rates of osteoarthritis in women appear to occur soon after the change of life. Regrettably, it can be tough to move through menopause, not least because of night sweats and other signs. So ladies, keep healthy and well, as this disease is also associated with the lack of estrogen. Menopause may play a role in the progression of osteoporosis. That's another problem as well. Of the few studies that measure this, most have found that higher bone mineral density is related to a greater incidence of osteoarthritis in the hips, hands, and knees.
What are the symptoms of arthritis that can help with its identification? Let's check it out. The knee is the part of the body most commonly affected by this problem, so in most cases, it will indicate a knee problem (knee osteoarthritis). Yet some people develop hip osteoarthritis, too. It is less prevalent but still important as a cause of disability besides knee disease. Then there is hand osteoarthritis which is painful and impairs essential motor functions. Instead, you already know that OA is a very complicated disease.
You should also remember that severely spreading or aggravating osteoarthritis is very individual. A subset of patients with knee OA have little change in pain or function with little structural progression. Others say, “No! It goes fast!”. So, who to believe? The trajectory of structural progression has little relationship to changes in pain and function. However, we do not know why this clinical course of the disease shows such variability. However, this might be what can take place during the disease process.
First, pain manifestations are prominent. This pain is exacerbated during activity and relieved during rest. Pain is also typically present late in the day or early evening but can also be noticeable in the early a.m., just after waking up from sleep. But not everyone has it the same way. Patients describe the difference in feeling the pain. Others describe the pain as dull and throbbing, and it has become more consistent over the years and is very much predictable.
On the other hand, some patients report that their pain is very vigorous and comes unexpected. Consequently, the pain can be psychologically distressing and inhibit the subject from engaging in everyday activities. This second, intense form of pain typically occurs with advanced disease.
A prolonged period of immobility can result in pain coupled with stiffness in the limbs. This makes it even less mobile. Joint locking can also occur unpredictably with the deterioration of the disease, and in particular, this is observed in the affected knee. Also, during the dislocation, noninflammatory effusions may develop.

Joint noise with movement in osteoarthritis is a strange symptom. Patients have described that sound as crackling, which sounds like breaking bones. Of course, patients are usually concerned about this when accompanied by pain. But bones are not broken. These weird noises are a sign of insufficiently maintained elements and materials that are the basic parts of joint cartilage.
Joint swelling and changes in the shape of joints are other classical features of the disease. It restricts your range of motion. This causes a feeling of instability among patients going through this. This overgrowth of bone situated around the joint area is a deformity caused by the disease. Deformities are snapped (lump) bump-ups around joint attachments. For instance, Heberden's nodules are the name of the specific nodular lesions found in people with hand osteoarthritis. Bony enlargement doctors can see upon examination.
Joint pain is the most commonly reported sign of osteoarthritis and what patients typically present to their doctor with. The diagnostician, however, has to dissect this pain during a history and physical. Examining the body is a key part of diagnosing a condition. All forms of osteoarthritis have pain and limitation of range of motion. Also, multiple professional medical exams are required for the complete identification of osteoarthritis. Imaging studies are crucial.
Some imaging studies have visualized changes in the joints. In the body, where no one can see, it is great that we can now view what is happening. Nevertheless, let's not forget the utility of simple radiography for diagnosis confirmation and exclusion of differentials. Also, imaging, especially CT or MRI, can provide us with useful information. To be fair, they are rarely required unless the diagnosis is a little bit dubious – and there is a significant suspicion of another etiology, such as meniscal damage. MRI is useful for studying neighboring extra-articular structures in patients with an uncertain diagnosis.

Lab tests are not generally needed to diagnose joint problems. However, they can also give crucial intelligence. For instance, evidence of arthritis or synovitis can be derived from immunological antibodies, increasing the likelihood of autoimmune arthritis. Measurement of uric acid levels is also suggested if gout is suspected. The chance of gout or autoimmune arthritis being the case may be so small that ordering some of those tests can lead to avoidable confusion due to false positives. This is why doctors seldom order point-of-care laboratory tests; they do not want to create problems unnecessarily.
Osteoarthritis may have a hereditary component, so such tests also hold significance. Now, diagnosticians use genetic tests that look for aberrations in collagen and other collagen matrix protein formation, leading to OA's early development. As joint pain is very common, you should understand and check whether it might be due to a hereditary disease. If a hereditary cause is detected in early infancy, it is easier to introduce preventive measures.
There are different types of osteoarthritis treatments you can go for. Patients may take medicines, but not only. Most importantly, the treatment should begin with the safest, least invasive therapies. Discover various methods for managing joint pain.
Doctors may suggest relevant physical activity. It is simple and noninvasive. A typical program consists of muscle strengthening and range-of-motion exercises. One benefit of exercise is that relief may occur quickly. So, it is worth working out! However, remember—it has to be a well-chosen exercise, preferably prescribed by a doctor or physiotherapist.
There are many different forms of physiotherapy. Regular, continuous exercise is key to weight loss, but it is difficult in patients with advanced disease. In such cases, swimming or cycling may come to the rescue. Therapeutic ultrasound is used for the treatment of osteoarthritis. Other non-pharmacologic interventions involve bracing and splinting to stabilize painful or unstable joints.
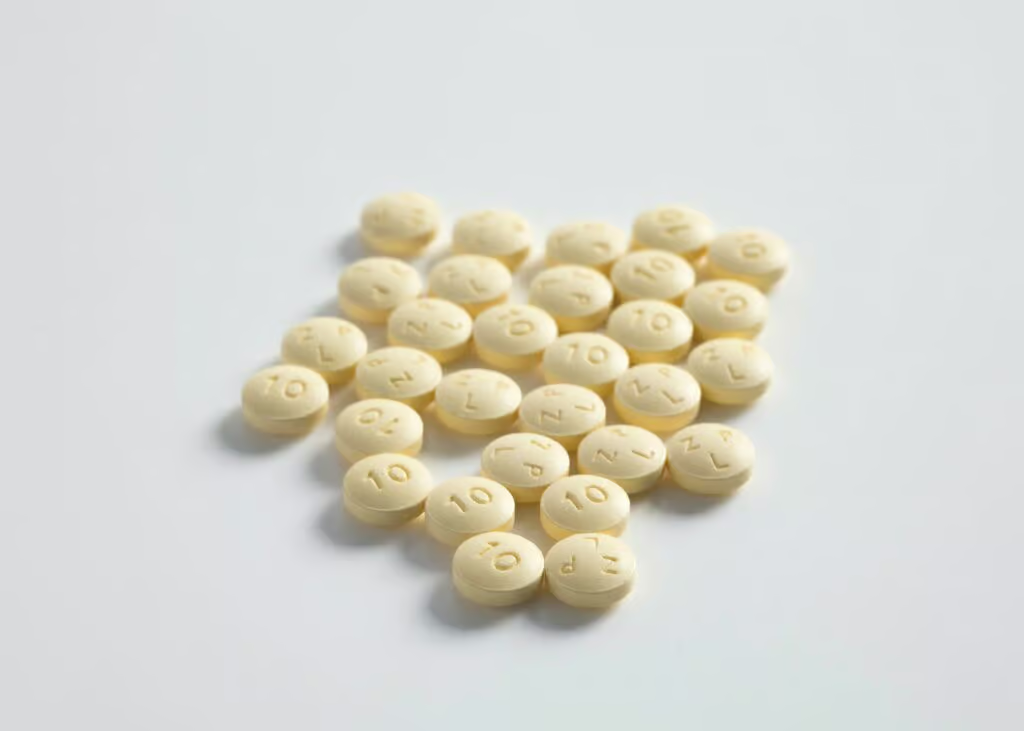
There are many other medications for osteoarthritis. Drugs are efficacious in alleviating disease symptomatology, particularly analgesics or pain relief. However, physicians must adhere to prescribed dosages to avoid liver damage. Sometimes, non-steroidal anti-inflammatory drugs (NSAIDs) will be used. You've probably taken these pills before, haven't you?
Pain often is treated with opioids, which has also been a possibility in treating osteoarthritis pain. Due to the risk of abuse, opioids should only be considered when treatment failure has occurred with other medications. But this is not the only option, of course.
Indications for surgical treatment should be strictly reserved for those in whom behavioral and pharmacological treatments have proven ineffective and pain and loss of function are intolerable. Total joint replacement is the most successful surgical option. Many prostheses and similar devices are available. The majority of prosthetic joints today can be used for years. This is optimistic news. The surgery, though invasive, provides a glimmer of hope for improved function when other avenues have not worked.
However, patients occasionally searched for other additional options. In these circumstances, pain has a great deal of incentive to seek other options. This means acupuncture is potentially effective in other areas, including chronic pain. Also, there are supplement formulas that also provide joint-supporting ingredients. On the other hand, spa therapy, mineral baths, and such are used and nonproblematic.
Table of Contents