They are also less numerous, with an average count of approximately 4,000 to 10,000 white blood cells per cubic millimeter of blood.

Types
White Blood Cells are a heterogeneous group of cells that differ in appearance and function. The first, most general division divides these cells into:
- Granulocytes (containing special granules, or granules, inside the cytoplasm)
- Agranulocytes (not containing granules)
Agranulocytes
In the category of agranulocytes, we identify lymphocytes, which are cells measuring between 6 to 15 micrometers in diameter and characterized by a large nucleus. Furthermore, they comprise approximately 25–35% of the total population of white blood cells. The primary function of lymphocytes is to recognize, identify, and eliminate foreign antigens, such as hostile cells or specific proteins on their surfaces. Lymphocytes are primarily produced in the red bone marrow but are also generated in the thymus, lymph nodes, spleen, and lymphatic nodules found on mucous membranes.
In terms of their functions, we can divide lymphocytes into:
- T lymphocytes – the most numerous group of lymphocytes (including subtypes of lymphocytes: Tc, Th, Treg, NKT) responsible for inducing cellular immunity and producing cytokines.
- B lymphocytes – they recognize the correct antigen and produce antibodies, thanks to which we become immune to a past infection. More than half of the lymphocytes are located in the lymphatic organs. The rest circulates the body – in the blood and connective tissue for antigens.
- Monocytes are the largest type of leukocytes, measuring between 10 to 40 µm. They are mostly created in the bone marrow and makeup about 3 to 8 percent of all leukocytes. One of their key properties is that they are phagocytic, meaning they can actively engulf and absorb fragments of dead tissue and pathogens in the blood. Monocytes can also move quickly; during inflammation, they can penetrate the endothelium of blood vessels and migrate to the sites of infection. Additionally, they secrete various cytokines, such as interferons and interleukins, which help regulate and mediate different stages of the immune response. Furthermore, once mature, monocytes that leave the bloodstream and enter tissues become macrophages.
Granulocytes
Granulocytes, in turn, can be divided into neutrophils, eosinophils, and basophils.
Neutrophils
Neutrophils (neutrophil granulocytes) are the most numerous granulocytes, constituting about 50 to 75 percent of all white blood cells. These cells are spherical and have a diameter of 12 to 15 µm. They are the main pillar of non-specific immunity, i.e., the body’s first barrier against harmful microorganisms, independent of antibody production. Neutrophils are made in the bone marrow, from where they enter the blood. In response to pro-inflammatory signals, they can also penetrate the walls of vessels into the tissues, where, after activation, they phagocytize pathogens. Moreover, they are the main component of pus produced in the acute phase of inflammation.
Eosinophils
Eosinophils (eosinophilic granulocytes) constitute an average of 1 to 5 percent of all white blood cells but percentage can change under the influence of stress, physical exertion, and even the time of day or phase of the menstrual cycle in women. Their name comes from the name of eosin (a dye popularly used in histology), which has an acidic nature and stains the internal granules of eosinophils red. Like neutrophils, eosinophils are also made in the bone marrow, and after maturation, they enter the blood. Furthermore, on the surface of eosinophils, many receptor proteins are “cooperating” with numerous interleukins and chemokines of the immune cascade. These cells are also phagocytes, and their role is to destroy parasites and allergens.
Basophils
Basophils (basophilic granulocytes) are spherical cells with an elongated nucleus with a diameter of about 10 µm, in terms of numbers. They constitute only about 1 percent of all white blood cells. Furthermore, they are produced in the bone marrow. Although neutrophils can phagocytose, it is not as efficient as neutrophils. Their “weapon” is the presence of specific substances in the granules: heparin, histamine, leukotrienes, and interleukin-4, secreted during the inflammatory process. It is the histamine released by basophils that causes blood vessels to dilate, which is the cause of the typical symptoms of allergies that many of us suffer from: swelling, redness, or a feeling of heat.
Function
In this case, it is worth discussing the function of individual white blood cells.
Granulocytes
Neutrophils are produced in larger quantities as a response to ongoing inflammation. They are attracted to the infected area by bacterial products. When bacteria bind to the receptors on the neutrophil cell membranes, it triggers exocytosis and an event known as the oxygen burst. Increased movement enhances the rapid absorption of bacteria through the process of endocytosis.
Basophils also migrate into tissues where they secrete proteins and cytokines. What sets them apart from other cells is their content of histamine and heparin, which are essential for inducing immediate hypersensitivity reactions. Moreover, these responses can differ in severity, ranging from mild hives (urticaria) to anaphylactic shock.
Eosinophils release substances that promote inflammatory processes, and they also can kill attacking microorganisms. They are particularly abundant in the mucous membranes of the digestive system, where they play a defensive role against parasites. Eosinophils can also be in large numbers in the mucous membranes of the respiratory and urinary systems. The number of circulating eosinophils tends to increase during allergic conditions, such as asthma.
Lymphocytes
Lymphocytes are classified into three main groups: T lymphocytes, B lymphocytes, and natural killer (NK) cells. All of these cells can recognize antigens due to the unique molecules present on their surfaces. This ability to recognize antigens is innate and develops without prior exposure to them.
When an antigen first enters the body, it binds directly to the receptor of the corresponding B lymphocyte. However, a complete immune response requires interaction between B lymphocytes and T lymphocytes. For T lymphocytes, the antigen is taken up by antigen-presenting cells, which digest it partially.
B lymphocytes, in turn, produce five types of antibodies that assist in neutralizing pathogens.
NK cells primarily focus on destroying harmful microorganisms and removing infected or cancerous cells through a process called phagocytosis. They accomplish this, among other things, by producing specific proteins. These cells have cytotoxic properties, allowing them to target and eliminate both viruses and cancer cells effectively.
Monocytes
After leaving the bone marrow, the place of their synthesis, monocytes go to the endothelium of blood vessels. They can pass into the tissues, where they turn into macrophages. Macrophages are activated by lymphokines from T lymphocytes. Activated macrophages migrate in response to a chemotactic stimulus, then engulf and kill bacteria in a process similar to the action of neutrophils. They play a key role in the body’s immunity, secreting almost 100 different substances, including factors that initiate coagulation.
Indications For Testing
Many factors affect the white blood cells count, but clear deviations from the norm may be the first symptom of many diseases.
Without a doubt, a leukocyte count (which is a component of a basic blood test) should be performed in the following cases:
- Suspected inflammatory diseases
- Suspected autoimmune and systemic diseases (e.g., lupus erythematosus, rheumatoid arthritis)
- Acute infections
- Allergies
- Suspected diseases associated with decreased immunity (e.g., AIDS or cancer)
- Regular checks of general health

What Does A Leukocyte Test Look Like?
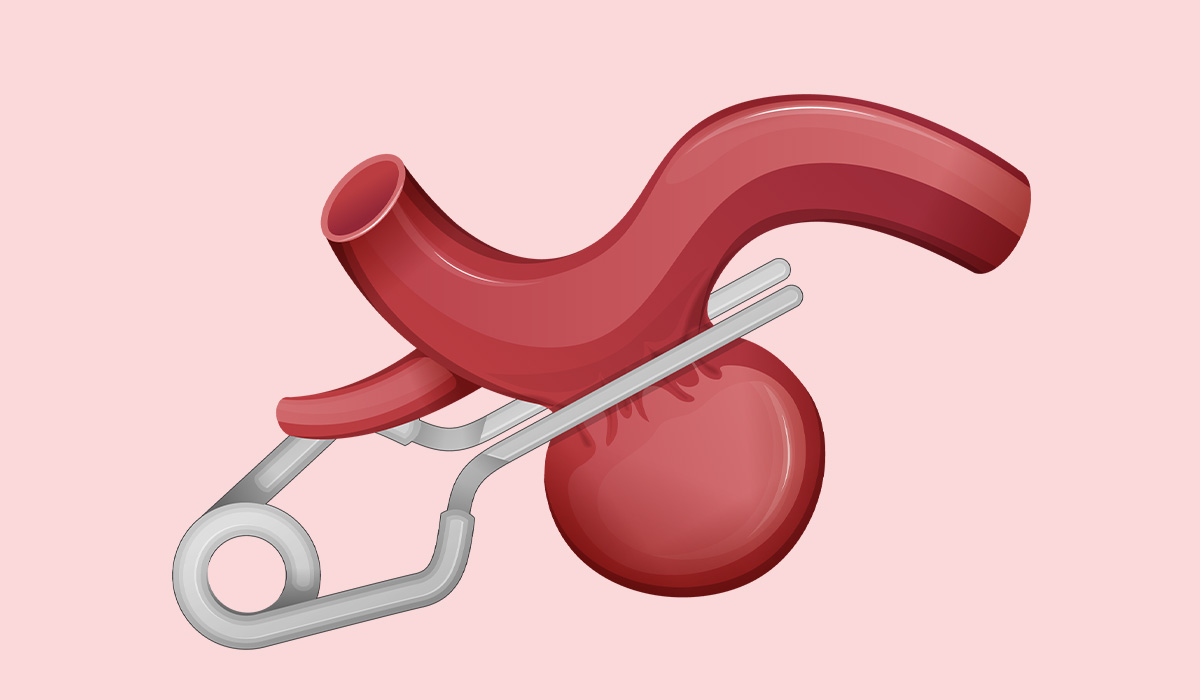
The process for a white blood cells test is comparable to that of a typical blood test. The blood sample is taken from a vein, usually at the inner elbow (antecubital fossa). In some cases, it may be drawn from the back of the hand, the foot, or a finger in children. A disposable needle is used to puncture the vein, and the blood is collected in a test tube.
It is important to arrive on an empty stomach for the sample collection in the morning. Before the test, ensure to notify the specialist about all medications you are currently taking, as certain medications can affect the test results. Additionally, notify the staff collecting the blood if you are carrying viruses such as HIV, HBV, or HCV or if you have a history of jaundice. This information helps ensure maximum safety and prevents the potential transmission of conditions.
Before inserting the needle, the person taking the blood will put a so-called tourniquet – this will allow the blood to accumulate in the vein and make it easier to collect. After removing the needle, press the injection site for a few minutes to control bleeding. After that, the sample will be analyzed in a special device. Blood test results are usually available on the same day.
Normal Leukocyte Count
In a healthy person, the norm for white blood cells should be in the range of 4000–11000/µl. In children, the number of white blood cells is slightly different, and changes occur with age:
- Newborns – 9000–30000/µl
- 1 year of life – 6000–20000/µl
- 4–6 years – 5000–15000/µl
- 10 years – 4500–13500/µl
The lymphocyte subpopulations listed above are presented as a percentage of the total number of white blood cells. The norm for individual forms for an adult is as follows:
- Neutrophils – 60–70%, 1800–8000 absolute cell count per µl. Younger forms (rods) constitute 3–5% of the number of white blood cells, while older forms (segmented) constitute 57–65%
- Eosinophils – 2–4%, in terms of absolute cell count per µl it is 50–400/µl
- Basophils – 0–1%, which is also presented in the number 10/µl300/µl
- Lymphocytes – 20–45%, or 1000–5000/µl
- Monocytes – 4–8%, or 30–800/µl
Consider the number of white blood cells (WBC) and their percentage picture in the diagnostics of suspected diseases. In some cases, the number of specific subpopulations increases, facilitating the diagnosis of the ongoing disease.
What Is Leukocytosis?
Leukocytosis is an increased level of white blood cells in the blood above standard. Leukocytes are, alongside erythrocytes (red blood cells) and thrombocytes (platelets), a key morphological element of blood. The main task of white blood cells is to protect the organism from pathogens. White blood cells consist of several types of blood cells listed below, giving their most characteristic functions.
Causes
Specialists identify several causes of leukocytosis, characterized by an excessively high white blood cell count. This increase is often linked to immune disorders, inflammation, bone marrow dysfunction (including myelodysplastic syndromes), post-hemorrhagic conditions, infections, tissue damage, metabolic disorders, certain medications, and proliferative diseases of the bone marrow and lymphatic system, such as myeloid and lymphatic leukemias. It’s also necessary to understand the inheritance patterns of leukemia.
Elevated white blood cell counts may sometimes be physiological rather than pathological. This condition, known as physiological leukocytosis, occurs when the number of white blood cells increases without underlying disease or inflammation. Examples include leukocytosis during pregnancy, which affects about 20% of healthy women, particularly in the third trimester; elevated leukocyte levels due to intense physical exercise; and increases following a meal, especially one high in protein. Additionally, fever can also cause an increase in white blood cell counts.
Patients often inquire about the impact of stress on leukocyte levels. Yes, prolonged exposure to stress can contribute to an increase in white blood cell counts.
However, leukocytosis is often associated with an elevated number of neutrophils. This condition is referred to as neutrophilia. It is most often a condition indicating:
- Acute and chronic bacterial, fungal, and viral infections, e.g., tuberculosis, shingles, chickenpox
- Autoimmune diseases
- AIDS
- Congenital neutrophil deficiency syndromes, familial neutrophil syndrome
- Neoplasms, especially carcinomas, soft tissue sarcomas
- Hypoxia
- Surgical procedures
- Heart attack, pulmonary embolism
- Injuries
- Burns
- Metabolic and endocrine diseases, such as hypothyroidism, gout, ketoacidosis
- Down syndrome
Symptoms
Leukocytosis itself does not manifest itself with any clinical symptoms. It can often go unnoticed until a blood test is performed. Symptoms are related to the ongoing disease, not the condition of elevated leukocytes.
What Is Leukopenia?
Leukopenia means a decrease in white blood cells below the established norm, i.e., 4 thousand cells/µl.
Leukocytes are blood cells produced in the bone marrow, spleen, lymph nodes, and thymus, which are responsible for the proper functioning of the immune system. The body can fight viruses, bacteria, and other pathogens thanks to them. Their deficiency increases the risk of developing serious infections, which can even end in death.
The largest group of leukocytes, accounting for 60-70 percent of all white blood cells, are neutrophils (also known as neutrophil granulocytes). Following them in abundance are lymphocytes.
The percentages of the remaining types of white blood cells are relatively small, e.g., eosinophils make up 2-4%, basophils comprise 0-1%, and monocytes account for 4-8%. Therefore, leukopenia is identified by a deficiency in neutrophils (a condition known as neutropenia) and lymphocytes.

Causes
Leukocyte deficiency is most often the result of a past infection. During the fight against it, leukocytes are used up, and the body needs some time to produce new ones, which may result in temporary leukopenia.
A complete lack of white blood cells or the presence of only a few is agranulocytosis, a life-threatening condition.
A low level of white blood cells can also be the result of various diseases, such as:
- Bone marrow diseases – bone marrow aplasia, bone marrow fibrosis, myelodysplastic syndromes, leukemia
- Cancers, e.g. Hodgkin’s lymphoma (malignant lymphoma)
- Autoimmune diseases – e.g., systemic lupus erythematosus, rheumatoid arthritis
- Hyperthyroidism
- Parasitic diseases
- Tuberculosis
- HIV/AIDS
- Hypersplenism (premature destruction of blood cells by the spleen)
- Kostmann’s syndrome (a congenital disorder involving reduced production of neutrophils)
Individuals who have recently undergone radiotherapy or chemotherapy may experience leukocytosis and increased white blood cell counts.
Low white blood cell counts can also be attributed to vitamin and mineral deficiencies, including folic acid, copper, and zinc.
Additionally, some medications—such as painkillers, antiepileptics, and certain psychotropic drugs—as well as medicine used to treat hyperthyroidism can contribute to the development of leukopenia. This condition may also arise from exposure to harmful chemical substances like varnishes, paints, organic solvents, benzene, and other aromatic hydrocarbons, particularly among individuals who encounter these substances in their professions.
Symptoms
People with the above symptoms require urgent hospitalization:
- Purulent skin lesions
- Low-grade fever or fever
- Enlarged cervical and submandibular lymph nodes
- Upper respiratory tract infections, e.g., tonsillitis or pneumonia
Leukopenia may also be accompanied by weakness, nausea and vomiting, and problems with concentration.
Sources
- Histology, White Blood Cell. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK563148/ - Agranulocyte. ScienceDirect.
https://www.sciencedirect.com/topics/immunology-and-microbiology/agranulocyte - Granulocytes. NIH.
https://www.ncbi.nlm.nih.gov/mesh?Db=mesh&Cmd=DetailsSearch&Term=%22Granulocytes%22%5BMeSH+Terms%5D - Histology, T-Cell Lymphocyte. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK535433/ - Histology, B-Cell Lymphocyte. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK560905/ - Histology, Monocytes. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK557618/ - Neutrophil: A Cell with Many Roles in Inflammation or Several Cell Types?. NIH.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5826082/ - Eosinophils from Physiology to Disease: A Comprehensive Review. NIH.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5829361/ - Role of Basophils in a Broad Spectrum of Disorders. NIH.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9186123/ - Lymphocytes and the Cellular Basis of Adaptive Immunity. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK26921/ - Natural Killer Cells: Development, Maturation, and Clinical Utilization. NIH.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6099181/ - Leukocyte Count. NIH.
https://www.ncbi.nlm.nih.gov/mesh?Db=mesh&Cmd=DetailsSearch&Term=%22Leukocyte+Count%22%5BMeSH+Terms%5D - Beyond Basic Blood Tests. NIH.
https://newsinhealth.nih.gov/2024/06/beyond-basic-blood-tests - Leukocytosis. NIH.
https://pubmed.ncbi.nlm.nih.gov/32809717/ - Low white blood cell count. NHS.
https://www.nhs.uk/conditions/low-white-blood-cell-count/
Eosinophils: What Are, Anatomy, Functions, and Conditions

Amyloidosis: What Is, Signs, Diagnosis, and Treatment

Biotin: What Is, Uses, Biotin Deficiency, and Dosing

Spondylosis: What Is, Causes, Complications, and Prognosis

Diabetes: What Is, Types, Symptoms, and Diagnosis
Aneurysm: What Is, Signs, Diagnosis, and Treatment

Vitamin B12: What Is, Functions, Deficiency, and Dosage

Vitamin B1
Edema: What Is, Causes, Diagnosis, and Treatment
Squamous Cell Carcinoma: What Is, Symptoms, and Treatment
Chromosome: What Is, Functions, Conditions, and How To Treat

Leg Pain: What Is, Causes, Symptoms, and Treatment

Diarrhea
H Pylori: What Is, Symptoms, Diagnosis, and Treatment
Hyperkalemia: What Is, Signs, Diagnosis, and Treatment